
Enteric Hyperoxaluria, an acquired metabolic disease
Enteric hyperoxaluria (EH) is a rare acquired metabolic disease in which patients accumulate unhealthy levels of oxalate, primarily in the urine and kidneys, causing irreversible damage to kidney tissue, severe and chronic kidney stone disease (multiple stones or multiple stone attacks), and lead to progressive kidney damage, chronic kidney disease (CKD) and end-stage kidney disease (ESKD).
Hyperoxaluria, high levels of oxalate in urine, is a relatively common condition in the U.S. population. It is estimated that up to 5 million people in the U.S. have been affected by hyperoxaluria and kidney stones. Of this 5 million people, it is estimated that 250,000 suffer from EH and kidney stones.
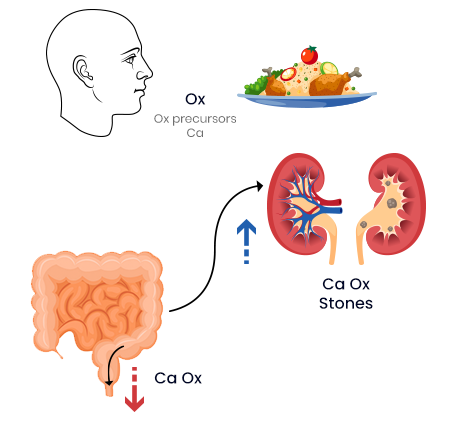
Oxalate is part of a normal diet, but the body views it as a toxic waste product and normally clears it via the gut or the kidneys. In enteric hyperoxaluria, the normal gut clearing mechanisms is not working, due to underlying gastrointestinal complications, causing the oxalate to reach dangerous levels. This oxalate accumulation is what can create chronic kidney stones, damage kidney tissue and cause kidney disease and more serious kidney diseases. There are currently no approved therapies to treat enteric hyperoxaluria.

Oxidien is developing a state-of-the-art oral enzyme, OX-1, for effective clearing of oxalate in the upper gastrointestinal tract. Clearing the is expected to reduce the oxalate accumulation in the kidneys and prevent associated kidney diseases.
Data to date suggest that OX-1 is very stable and active even in a harsh acidic environment, such as the human stomach, and that it has very high affinity for oxalate. This novel chemistry may also provide differentiation in clinical outcomes as a sachet form of OX-1 was well tolerated and showed statistically significant reduction of urinary oxalate (29%) at an initial low dose evaluated in healthy volunteers on a controlled diet. Oxidien is now in preparation to do a dose-finding study to evaluate higher doses in patients with enteric hyperoxaluria.
